Interoperability And Integration To Future Proof Healthcare

Interoperability And Integration To Future Proof Healthcare Ensuring interoperability across health and social care systems inevitably means that delays can be avoided, speeding up the patient’s time for treatment and care. by ‘joining the dots’ and linking nhs organisations through real time technology, we can move away from the typical historic siloed working practices, transforming care. Pros: red hat integration provides a suite of tools and technologies for healthcare interoperability, emphasizing open source solutions. their platform offers flexibility and customization options.
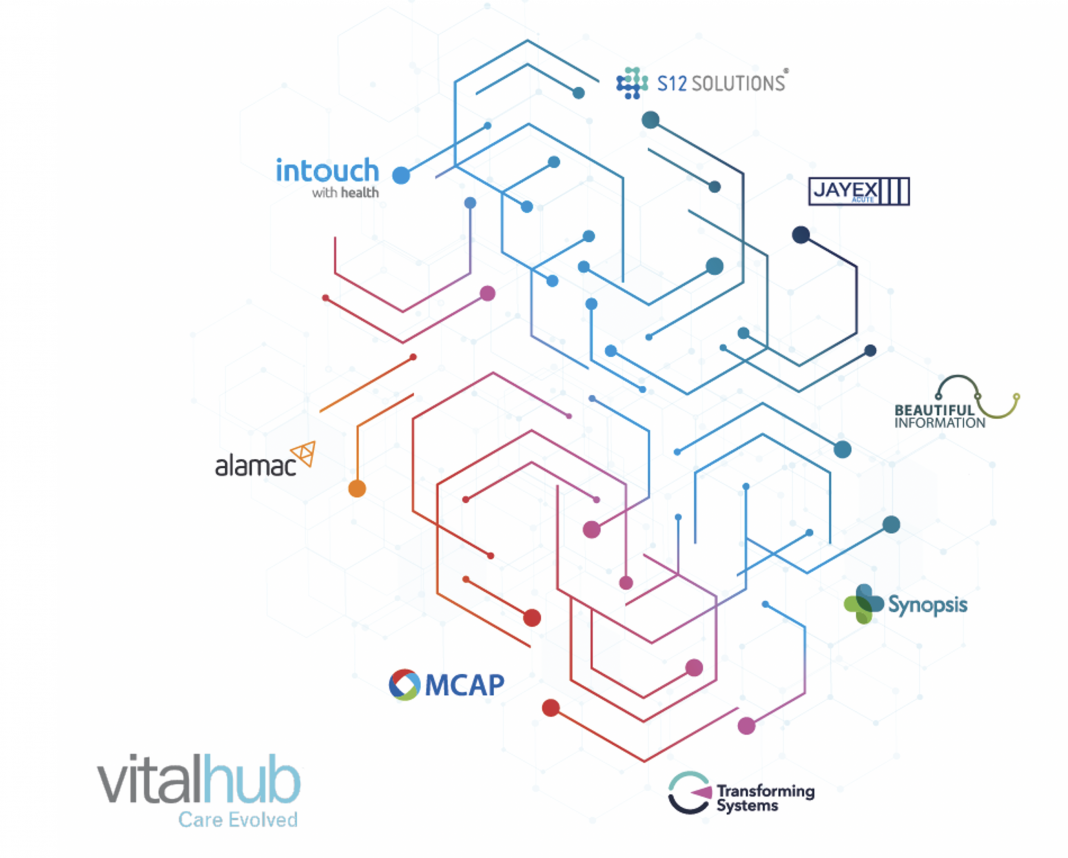
Interoperability And Integration To Future Proof Healthcare Interoperability seeks to remove barriers and breakdown silos to facilitate the exchange of health information, while still protecting individual privacy. the goal is to ensure that healthcare it systems can improve their ability to exchange, process and interpret shared health information between devices, applications and systems across the. Barriers to interoperability. in addition to deliberate attempts to block hie, other systemic barriers to interoperability exist despite attempts to address them via the hitech act and other reforms. one major barrier is lack of coordination among different facilities health systems participating in or facilitating hie (healthit.gov, 2019). Spurred by several policy initiatives, most notably the health information technology for economic and clinical health (hitech) act of 2009, health care in the united states has experienced a steeply upward adoption curve of electronic health records (ehr) technology. as of 2016, 96 percent of hospitals and 78 percent of physicians' offices were using certified technology for health care. Adoption of our recommendations will simplify the continual enhancement, maintenance, oversight and the analytical functions of a fully interoperable, public health and medical data system.

Interoperability And Integration To Future Proof Healthcare Spurred by several policy initiatives, most notably the health information technology for economic and clinical health (hitech) act of 2009, health care in the united states has experienced a steeply upward adoption curve of electronic health records (ehr) technology. as of 2016, 96 percent of hospitals and 78 percent of physicians' offices were using certified technology for health care. Adoption of our recommendations will simplify the continual enhancement, maintenance, oversight and the analytical functions of a fully interoperable, public health and medical data system. In this context, interoperability. refers to the ability of different medical devices, systems, and software applications to. communicate, exchange data, and work togeth er effectively [1. Healthcare stakeholders have largely achieved the goal of converting clinical and administrative information into digital formats through the wide scale implementation of electronic health records (ehrs). however, the ability to share semantically interoperable electronic health information (ehi) among organizations, patients, payers, and other stakeholders has remained limited. consequently.

Building A Future Proof Healthcare Data Interoperability Strategy In this context, interoperability. refers to the ability of different medical devices, systems, and software applications to. communicate, exchange data, and work togeth er effectively [1. Healthcare stakeholders have largely achieved the goal of converting clinical and administrative information into digital formats through the wide scale implementation of electronic health records (ehrs). however, the ability to share semantically interoperable electronic health information (ehi) among organizations, patients, payers, and other stakeholders has remained limited. consequently.

Comments are closed.